Thermography Articles
Why Mammography Screening is Being Abolished in Switzerland
Whether breast cancer screening does more harm than good has been debated extensively. Earlier this year the Swiss Medical Board published a report recommending that no new systematic mammography screening programs be introduced. Here is how and why they came to this conclusion. The Swiss Medical Board is part of an independent health technology assessment initiative in Switzerland. In 2013 they were asked to review the current mammography screening program. The team of experts on the board included amongst others, a medical ethicist, a clinical epidemiologist, a pharmacologist, an oncologic surgeon, a nurse scientist, a lawyer, and a health economist.
Whether breast cancer screening does more harm than good has been debated extensively. Earlier this year the Swiss Medical Board published a report recommending that no new systematic mammography screening programs be introduced. Here is how and why they came to this conclusion. The Swiss Medical Board is part of an independent health technology assessment initiative in Switzerland. In 2013 they were asked to review the current mammography screening program. The team of experts on the board included amongst others, a medical ethicist, a clinical epidemiologist, a pharmacologist, an oncologic surgeon, a nurse scientist, a lawyer, and a health economist.
“Systematic mammography screening” is the term generally used to describe the serial radiological examination of women within the framework of a screening program whereby all women in a specific age group are invited to an X-ray examination of their breasts which is not conducted by a doctor. At the time the country had in place a comprehensive screening program which was offered to all women aged from 50 to 69.
The board spend twelve months reviewing all available evidence and its implications. They reported becoming “increasingly concerned” about the widely believed notion that mammograms were safe and capable of saving lives. They said “As we embarked on the project, we were aware of the controversies that have surrounded mammography screening for the past 10 to 15 years. When we reviewed the available evidence and contemplated its implications in detail, however, we became increasingly concerned.” In fact they concluded that statistics clearly indicated that mammograms appeared to be preventing only 1 death per 1,000 women screened, and actually caused harm to many more. Their thorough review left them no choice but to recommend that “no new systematic mammography screening programs be introduced, and that a time limit should be placed on existing programs.”
The report was made public at the start of 2014 wherein they advised that the quality of mammography screening should be evaluated and every woman should be informed, in a “clear and balanced” way, about the benefits in addition to the potential harms of screening.(i) The subject of whether breast cancer screening in women with no symptoms has been questioned by many industry experts over the years and this revelation from the Swiss seems to prove that it no longer makes sense.
Two members of the Swiss Medical Board’s expert panel went on to expand on their research and the reasons which led to their conclusion in an article in New England Journal of Medicine (ii) discussing three major factors:
1. OUTDATED CLINICAL TRIALS “We noticed that the ongoing debate was based on a series of reanalysis of the same, predominantly outdated trials. The first trial started more than 50 years ago in New York City and the last trial in 1991 in the United Kingdom. None of these trials were initiated in the era of modern breast-cancer treatment, which has dramatically improved the prognosis of women with breast cancer. Could the modest benefit of mammography screening in terms of breast-cancer mortality that was shown in trials initiated between 1963 and 1991 still be detected in a trial conducted today?”
2. BENEFITS DID NOT OUTWEIGH THE HARMS The panel referred to a recent study published in The Lancet, recognized as one of the largest and longest studies of mammography to date. This study involved 90,000 women who were followed for a period of 25 years. The study concluded that mammograms have absolutely NO impact on breast cancer mortality (iii). These conclusions were widely publicized at the time and showed that the death rate from breast cancer was virtually identical between those who received an annual mammogram and those who did not, while 22% of screen-detected invasive breast cancers were over-diagnosed, leading to unnecessary treatment.
The Swiss experts stated: “This means that 106 of the 44,925 healthy women in the screening group were diagnosed with and treated for breast cancer unnecessarily, which resulted in needless surgical interventions, radiotherapy, chemotherapy, or some combination of these therapies. In the best case, the small reduction in breast-cancer deaths was attenuated by deaths from other causes. In the worst case, the reduction was canceled out by deaths caused by coexisting conditions or by the harms of screening and associated overtreatment. Did the available evidence, taken together, indicate that mammography screening indeed benefits women?”
This concurs with the Cochrane Collaboration Review, published in 2013 which also found no evidence that mammography screening has an effect on overall mortality (v). Thus calling into question whether mammography screening really benefits women. According to the authors of the Cochrane review: “If we assume that screening reduces breast cancer mortality by 15% and that over diagnosis and overtreatment is at 30%, it means that for every 2000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.”
3. WOMEN’S PERCEPTIONS OF MAMMOGRAPHY BENEFITS ARE NOT MIRRORED IN THE REALITY The Swiss panel said “we were disconcerted by the pronounced discrepancy between women’s perceptions of the benefits of mammography screening and the benefits to be expected in reality.” One survey found that the majority of women believed that mammography screening programs reduced the risk of breast cancer deaths by at least half and prevented at least 80 deaths per 1,000 women screened (vi). In this survey, which involved more than 4000 participants, most women said they believed mammography reduced the risk of breast cancer deaths by at least half and prevented at least 80 deaths per 1,000 women screened. The authors concluded that “Misconceptions were widespread: a majority of women believed that screening prevents or reduces the risk of contracting breast cancer (68%), that screening at least halves breast cancer mortality (62%), and that 10 years of regular screening will prevent 10 or more breast cancer deaths per 1000 women (75%).”
However in reality, mammography may, at best, offer a relative risk reduction of 20 percent and prevent in absolute terms only one breast-cancer death per 10,000 women. This led to the panel of experts to ask a long overdue question: “How can women make an informed decision if they overestimate the benefit of mammography so grossly?”
In conclusion the Swiss said “It is easy to promote mammography screening if the majority of women believe that it prevents or reduces the risk of getting breast cancer and saves many lives through early detection of aggressive tumors.4 We would be in favor of mammography screening if these beliefs were valid. Unfortunately, they are not, and we believe that women need to be told so. From an ethical perspective, a public health program that does not clearly produce more benefits than harms is hard to justify. Providing clear, unbiased information, promoting appropriate care, and preventing over diagnosis and overtreatment would be a better choice.”
Often women can feel almost guilt-tripped into thinking that skipping their annual mammogram appointment is hugely irresponsible. The industry over the years talked about it as a one size all type of approach to preventing or detecting breast cancer. In reality there are now reasonable doubts regarding symptom free women. We expect our health professionals to know what they’re talking about, and to give the best advice possible. But this research suggests that doctors can be just as confused and misinformed as the patients, compounded by misinformation and media propaganda in a powerful and profits driven industry which often chooses to dismiss research that dramatically contradicts their profit-based agenda.
The industry as a whole has a responsibility to no longer ignore mounting research showing that more women are being harmed by regular mammograms than are saved by them.
OTHER POINTS MAKING MAMMOGRAMS RISKIER AND UNRELIABLE: The Swiss medical board found that for EVERY BREAST CANCER DEATH PREVENTED in US women over a 10-year course of annual screening beginning at 50 years of age:
- 490 to 670 women are likely to have a false positive mammogram with repeat examination.
- 70 to 100 forced to undergo an unnecessary biopsy.
- 3 to 14 women have an over-diagnosed breast cancer that would never have become clinically apparent and present no danger.
In addition studies also indicate that up to 50 percent of women have dense breast tissue, making mammograms very difficult to decipher. Dense breast tissue and cancer can both appear as white areas on an X-ray, therefore making it nigh impossible for a radiologist to detect cancer in these women with any level of accuracy. This has led to legislation, or ‘breast density laws’, to be passed in California, Connecticut, New York, Virginia, and Texas, which make it absolutely mandatory for radiologists to inform their patients who have dense breast tissue that mammograms are basically useless for them. A law is currently being considered at a federal level so all women are informed across the country.
WOMEN CARRYING THE BRCA 1 or 2 GENE: Women who have this genetic mutation are known to have an increased risk of breast cancer and in the past have often been encouraged to have regular mammograms. However research published in the British Medical Journal(BMJ) in 2012 studied the risk of breast cancer associated with diagnostic radiation in carriers of BRCA1/2 mutations (vii). This research covered almost 2000 women in Britain, France and the Netherlands. They found that women carrying this mutation are particularly vulnerable to radiation-induced cancer stating that women carrying this mutation who were exposed to diagnostic radiation before the age of 30 were twice as likely to develop breast cancer, compared to those who did not have the mutated gene.
They also found that the radiation-induced cancer was dose-responsive, meaning the higher the dose, the greater the risk of cancer developing. The authors concluded that: “The results of this study support the use of non-ionizing radiation imaging techniques (such as magnetic resonance imaging) as the main tool for surveillance in young women with BRCA1/2 mutations.”
Incredibly, despite these findings, the National Cancer Institute reports that some expert groups still recommend women with BRCA 1/2 mutation undergo a mammogram every year starting as young as age 25 (viii) – the exact scenario that the BMJ study found may double their breast cancer risk!
Be informed, be confident that your doctor is fully educated with all studies and make your own decision. Women need to know that there are other screening options (including thermography, ultrasound, and/or MRI), each with their own strengths and weaknesses, and you have a right to utilize those options. Know your breasts and seek advice should you notice any changes. Also remember that we can minimize the risk of breast cancer by focusing attention on prevention in addition early detection.
Eat a healthy diet full of fresh organic vegetables and avoid sugar and processed foods. Include organic animal based sources of omega 3 fatty acids. Reduce alcohol intake. Exercise regularly and maintain a healthy body weight. Be informed. Remain informed.
REFERENCES/SOURCES:
- (i) Systematic Mammography Screening by The Swiss Medical Board
- (ii) http://www.nejm.org/doi/full/10.1056/NEJMp1401875?af=R&rss=currentIssue&&
- (iv) http://www.ncbi.nlm.nih.gov/pubmed/24519768?dopt=Abstract
- (iii) http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)61611-0/fulltext
- (v) http://www.ncbi.nlm.nih.gov/pubmed/23737396?dopt=Abstract
- (vi) http://ije.oxfordjournals.org/content/32/5/816
- (vii) http://www.bmj.com/content/345/bmj.e5660
- (viii) http://www.cancer.gov/cancertopics/factsheet/Risk/BRCA
- (ix) http://www.naturalcuresnotmedicine.com/2014/07/top-2-food-additives-stealing-yearslife.html
What makes Thermography so different from other medical imaging technologies?
What most of us are accustomed to when we think of medical imaging is the use of X-ray, CT, MRI, or ultrasound. All of these imaging tools are considered structural imaging technologies; they look inside the body for structural changes such as broken bones, tumors, damage to organs, etc. What separates these technologies from infrared imaging is that Thermography detects infrared (heat) markers that reflect the body’s subtle underlying chemical and nervous system signals. This allows us to look at how the body is functioning. These neurochemical signals may be the only sign that a problem exists, a remnant of injury indicating that healing has not finished, or a signal sent in advance of significant damage to the body. With this information in hand, you and your health care provider can outline a method for treating a current problem or possibly preventing future problems before they cause irreversible damage.
What most of us are accustomed to when we think of medical imaging is the use of X-ray, CT, MRI, or ultrasound. All of these imaging tools are considered structural imaging technologies; they look inside the body for structural changes such as broken bones, tumors, damage to organs, etc. What separates these technologies from infrared imaging is that Thermography detects infrared (heat) markers that reflect the body’s subtle underlying chemical and nervous system signals. This allows us to look at how the body is functioning. These neurochemical signals may be the only sign that a problem exists, a remnant of injury indicating that healing has not finished, or a signal sent in advance of significant damage to the body. With this information in hand, you and your health care provider can outline a method for treating a current problem or possibly preventing future problems before they cause irreversible damage.
Many patients are also confused with regard to their condition. For example, patients with chronic pain who have had treatment with little or no relief may have been treated for the wrong condition. Infrared imaging has helped many patients get to the cause of their condition so that proper treatment can be rendered.
The applications of Thermography are broad and range from simple soft tissue injury to a risk assessment marker for breast cancer. It is important to note that infrared imaging, like other imaging procedures (e.g. CT, MRI, mammography, ultrasound) does not provide a diagnosis. Infrared imaging cannot be used as a "body scan" to search for metastasis (the spread of cancer) or internal organ pathologies. Infrared imaging is an additional procedure that your doctor can use along with other tests to evaluate your health. Only your physician can provide you with a diagnosis. The following list is just some of the conditions that have associated infrared thermal emission markers:
- Altered gait manifestations
- Arteriosclerosis (peripheral)
- Brachial Plexus Injury
- Breast Disease Bursitis
- Carotid Artery Stenosis
- Carpal Tunnel Syndrome
- Chronic pain
- Compartment Syndromes
- Complex Regional Pain Syndrome (CRPS)
- Dental Irritation/Inflammation
- Diabetes (secondary complications)
- Disc Syndromes (spinal discogenic pain)
- Facet Syndrome
- Fibromyalgia
- Headache Evaluation (e.g. cervicogenic, migraine, sinus)
- Herniated Disc/Ruptured Disc
- Hypesthesia
- Hyperaesthesia
- Inflammation
- Intervertebral Disc Disease
- Ligament Tears
- Lumbosacral Plexus Injury
- Muscular Spasm
- Muscle Tears
- Myofascial Irritation
- Myofascial Pain Syndrome
- Nerve Entrapment
- Nerve Impingement/Pressure
- Nerve Root Irritation
- Nerve Stretch Injury
- Neuritis
- Neuropathy
- Neurovascular Compression
- Osteoarthritis
- Paresthesia
- Peripheral Nerve Abnormalities
- Pinched Nerves
- Referred Pain Syndromes
- Reflex Sympathetic Dystrophy (RSD)
- Repetitive Strain Injuries
- Raynaud’s Disease
- Rheumatoid Arthritis
- Sacroiliac Ligament Tear
- Sacroiliac Syndrome
- Sensory Nerve Abnormalities
- Sinus Irritation/Inflammation
- Skin Conditions
- Soft Tissue Injury
- Spinal Cord Injury
- Sports Injuries
- Strain/Sprains
- Superficial Vascular Disease
- Synovitis
- Temporal Arteritis
- Tendonitis
- Thoracic Outlet Syndrome
- Thyroid Conditions
- TMJ Dysfunction (TMD)
- Trigeminal Neuralgia
- Trigger Points
- Whiplash Conditions
- And many more …
Sources: Index Medicus - J Thermology, Acta Thermographica, J Breast
United Breast Cancer Foundation
Did you know that The United Breast Cancer Foundation offers free or low cost breast screenings to women and men nationwide! UBCF covers various screening technologies such as thermography, ultrasound, and mammograms. The program is open to all regardless of age, race, gender, income, or medical insurance. Check it out at www.ubcf.org.
Breast Thermography- A Responsible Second Look
Breast cancer and other breast diseases have become a tremendous issue in women's health today, particularly in advanced industrialized nations. Also note that approximately 1,000 men get breast cancer yearly.
Breast cancer and other breast diseases have become a tremendous issue in women's health today, particularly in advanced industrialized nations. Also note that approximately 1,000 men get breast cancer yearly.
A procedure which has gone largely unnoticed is Breast Thermography, also known as Breast Thermal Imaging. Breast thermography promises the opportunity of earlier detection of breast disease than has been possible with breast self examination, physician palpation, or mammography.
The medical community investigated breast thermography quite extensively during the late 1970's and early 1980's. The FDA approved the procedure as an adjunctive tool in breast cancer screening, and many physicians, concerned about the radiation exposure of mammography, began to promote thermography as a replacement for mammography. This was error.
Basics of Thermal Imaging
Thermography is a non invasive test. This means that it sends nothing into your body. In fact, there is no contact with the body of any kind, no radiation and the procedure is painless.
Utilizing very sophisticated infra-red cameras and desk top computers, thermal imaging technicians simply capture a photograph of the breasts. An infra-red photograph, or heat picture. The data is stored in a computer and then can either be printed on high resolution color printers, or sent electronically to a physician with a similar computer for analysis.
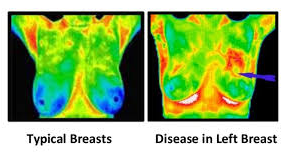
The physician, such as a radiologist or thermal imaging specialist, then compares the heat patterns in the left breast to the right breast. Any difference in heat, or any specific blood vessel patterns in one breast that do not appear in another indicate a physiologic abnormality. This may be pathological (a disease) or it might indicate an anatomical variant. When a thermogram is positive, the job of differential diagnosis begins.
This is all that thermal imaging, or thermography provides. A physiologic marker that some abnormality is present in the breast. Nothing more and nothing less. This is however, an extremely valuable and important finding, but it has historically been the interpretation of these findings that has been the problem, and is now the subject of the "responsible second look".
Competition Paradox with Mammography
Scientists and health care researchers have been looking for many decades at tools that can identify breast cancer reliably and quickly. It takes years for a tumor to grow, and the earliest possible indication of abnormality is needed to allow for the earliest possible treatment and intervention.
Thermography was viewed as a possible early diagnostic tool for cancer. The reason I stated that this was error, is quite obvious, but almost totally overlooked by the clinicians and researchers of the day.
Thermography is a test of PHYSIOLOGY. It does not look at anatomy or structure, and it only reads the infra-red heat radiating from the surface of the body.
Mammography, on the other hand, is a test of ANATOMY. It looks at structure. When a tumor has grown to a size that is large enough, and dense enough to block an x-ray beam, it produces an image on the x-ray or mammographic plate, that can be detected by a trained radiologist. A fine needle biopsy is then generally performed to identify the type of tissue in the mass, to determine if atypical or cancerous cells are present.
We now come to an important point. Neither thermography nor mammography can diagnose breast cancer. They are both diagnostic tests which reveal different aspects of the disease process and allow for further exploration.
The problem has been, that a number of studies were done on patients who had an established diagnosis of breast cancer. These studies were done with thermal imaging, wherein the patient having known breast cancer acted as their own controls.
In other words, the patients cancerous breast was compared thermographically to the patients healthy breast. In nearly every case the cancerous breasts were hotter and had specific patterns of heat mimicking the appearance of blood vessels that suggested 1) cancerous tumors were hotter than surrounding tissue and 2) blood vessels in the vicinity of the tumor were engorged with blood and this produced hotter thermal images than the normal vessels in the opposite breast.
This made complete sense, until the research proceeded to look at younger, and younger women.. It was at this time thermography was viewed as a failure. In a local newspaper article in my home town paper covering my clinic, the caption read "Thermal Imaging...Useful tool or dinosaur in breast cancer detection".
Here is the problem. Early stage tumors have not grown large enough or dense (thick) enough to be seen by current mammography. When the thermogram picks up the heat from the tumor, a mammogram is performed and often the mass is not detected.
The result of the thermogram is then considered a "False Positive". The more patients of younger age screened with the so-called false positive, the more suspicion was placed on thermography.
Eventually lobbying efforts at the AMA's House of Delegates and at Medicare, brought about the removal of thermographic coverage by insurance companies, and the demise of thermography in large measure. This is most unfortunate.
Thermography was viewed as a competitive tool to mammography, a role for which it was never intended. This is a known fact in the community of board certified clinical thermographers. Thermography is complimentary to mammography and an adjunctive tool in the war on breast cancer. We must learn to accept the information these tools bring to us, and use the information to the best management of the patient. You and me.
The Correct Role for Thermal Imaging
This is where the correct utilization of thermographic imaging will demonstrate it's ability. In the correct model, thermography of the human breast can make a profound and positive impact on breast cancer and other breast disease. Here's the correct model.
Thermography is a risk marker for breast pathology. This paper is written for the general public and I am not going to burden the reader with a large base of complex studies that have been published demonstrating the clinical utility and reliability of the procedure. Suffice it to say it is overwhelming.
My purpose is to identify the role of thermography. It is actually quite a simple one.
In performing this procedure, which is non-invasive and non-compressive, we can establish a baseline in women as young as 18. Yearly thermographic evaluations as part of a routine annual physical can be performed inexpensively and quickly.
As soon a suspicious (positive) breast thermal examination is performed, the appropriate followup diagnostic and clinical testing can be ordered. This would include mammography and other imaging tests, clinical laboratory procedures, nutritional and lifestyle evaluation and training in breast self examination.
With this protocol, cancer will be detected at its earliest possible occurrence, It has been estimated by a number of my colleagues that thermography is correct 8-10 years before mammography can detect a mass.
This is both exciting and frustrating for the clinician and the patient. It is exciting as it gives us the opportunity to intervene long before cancer can grab hold of the body. Cancer is opportunistic. We must find it, or the suspicious signs of its' presence long before the intervention stage has passed.
On the other hand, it is frightening to uneducated clinicians and patients, and poses quite a dilemma for those rooted in the "wait and see" attitude. It is very difficult to sit in front of a patient and tell them that you have a positive finding with a procedure that suggest the possibility of a terrible disease, and then have no other tools available to confirm or deny the tests correctness.
This is not thermography's failure. Indeed this is where the scientific and research community has failed thermal imaging.
If one can grasp the simple concept that thermography is detecting the fever of a breast pathology, whether it is cancer, fibrocystic disease, an infection or a vascular disease, then one can plan accordingly. One can lay out a careful clinical program to further diagnose and or MONITOR the patient until other standard testing becomes positive, thus allowing for the earliest possible treatment.
Two other positive benefits of breast thermal imaging have also been proposed by the author at scientific symposia. As a non-invasive low cost procedure, thermography can be made available to two distinct subpopulations:
- Patients who are economically deprived and can not afford the cost of mammography.
- Patients who are afraid of mammography due to fear of x-ray or breast compression, and thus do not get their recommended mammogram.
The Paradigm Shift
It is my position that the role of thermography is vastly different than it originally was determined to be. We must begin to look at this tool for what it really is. A highly accurate, high yield thermometer, much like the one every physician uses daily to determine the presence of fever.
Numerous studies have been published in the United States, England and France demonstrating that patients in the false positive thermographic group I mentioned earlier, those patients with positive thermograms and negative mammograms who were told the thermography was wrong, were determined by long term follow-up to have developed breast cancer in exactly the location thermography had demonstrated its positive finding 5-10 years earlier.
Thermography's only error is that it is too right ~ too early. It is our job as scientists, physicians and concerned patients, to identify the appropriate protocols once a thermogram is positive. It is in this capacity that the paradigm must shift.
We have a wonderful and exciting opportunity to at last change the incidence of this horrible disease, by screening younger women utilizing high resolution thermal imaging technology and then placing those women with positive findings into the appropriate lifestyle modification and treatment model which may be able to prevent or minimize not only cancer, but all breast disease.
This is our task.
Written by: William Cockburn, D.C., D.A.B.F.E., F.I.A.C.T
Positive comparative study showing changes over one year
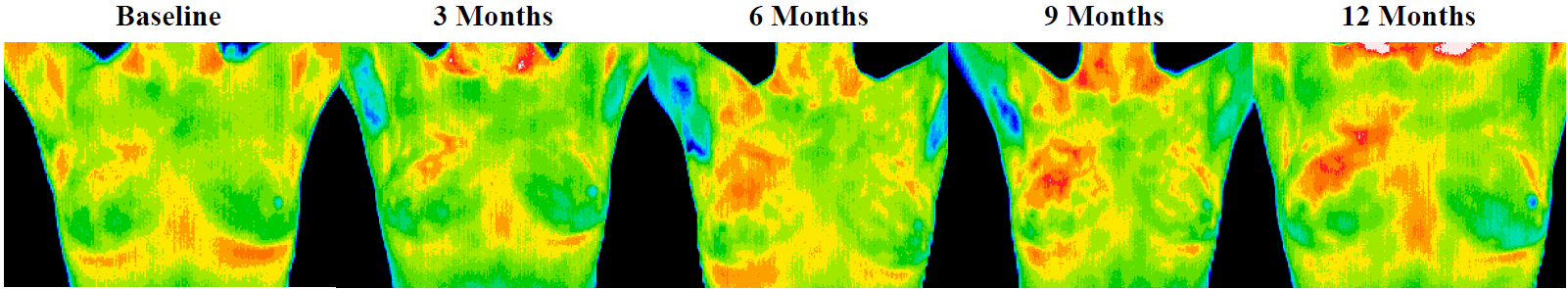
This patient was also age 37 when her first baseline thermogram showed a slight hyperthermic asymmetry in the upper right breast. The follow-up study showed the pattern had become more well defined and although clinical correlation did not find anything remarkable it was decided to repeat the exam again in a further 3 months, when again significant changes were seen. Mammography was performed at this stage with the thermographic guidance of the locally suspicious area at 1 O’clock to the right nipple. The mammographic findings were inconclusive and the patient was referred for a repeat mammogram in 12 months. Thermographic monitoring was continued and at the fifth comparative study at 12 months significant changes were still evident and the hyperthermic asymmetry (temperature differentials) had increased. Immediate further investigation was strongly recommended despite a scheduled mammogram in 6 months, and at the patients insistence a repeat mammogram was performed which clearly showed a small calcification (1 mm) at 1 O’clock. Within one week a lumpectomy had been performed with good margins and the pathology confirmed as a malignant carcinoma (DCIS).
This patient has now had stable thermograms for the last 2 years and is expected to remain healthy.
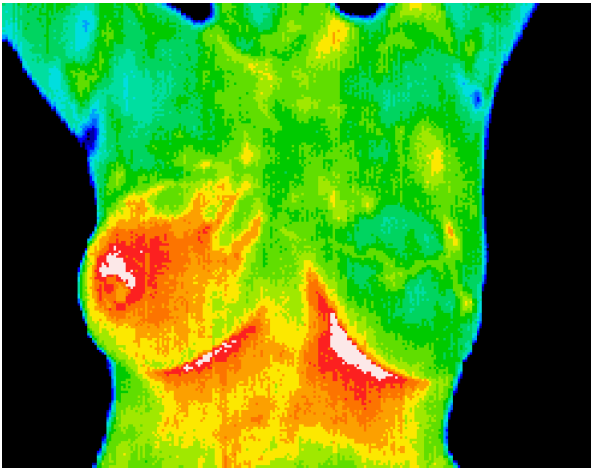 Inflammatory
Breast Disease
Inflammatory
Breast Disease
The results of this routine study led to the diagnosis of inflammatory carcinoma in the right breast. There were no clinical indications at this stage. (Thermography can show significant indicators several months before any of the clinical signs of inflammatory breast disease, skin discoloration, swelling and pain). Inflammatory breast disease cannot be detected by mammography and is most commonly seen in younger women, the prognosis is always poor. Early detection provides the best hope of survival.
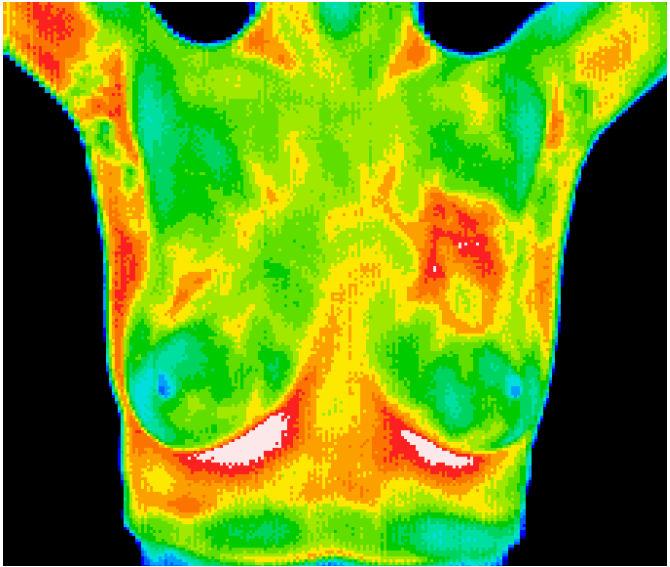 DCIS with accompanying
angiogenesis
DCIS with accompanying
angiogenesis
This 37 year old patient presented for routine thermographic breast screening, she was not in a high risk category and had no family history. No breast exams had been performed previously. The vascular asymmetry in the upper left breast and the local hypothermia at 11 O’clock was particularly suspicious and subsequent clinical investigation indicated a palpable mass at the position indicated. A biopsy was performed and a DCIS of 2 cm was diagnosed.
Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer
Digital infrared thermal imaging (DITI) has resurfaced in this era of modernized computer technology. Its role in the detection of breast cancer is evaluated.
